

Elevating health benefits with integrated virtual care
From primary care to chronic condition support, an integrated virtual care benefit can seamlessly connect an entire population to the care they need.
A recent Harris Poll of more than 2,500 Americans explored the varied healthcare experiences and obstacles people face when they try to take care of themselves or a loved one.
Among the findings was the revelation that 65% of adults believe their health would improve if they regularly worked with a trusted healthcare provider. Echoing this sentiment, benefit leaders at mid- and large-sized employers polled by Teladoc Health in 2023 overwhelmingly agreed that an integrated, whole-person approach to care would improve the healthcare experience and build a better benefits package.
However, the current state of care still relies on a fragmented collection of point solutions that contributes to frustrating inefficiency, complexity and inconsistent care, and administrative burden for benefit managers. That may be why 73% of respondents in the Teladoc Health survey anticipate evaluating virtual care vendor consolidation in 2024.
Integrating virtual primary care and general medical services with virtual chronic condition support for diabetes, high blood pressure, obesity and mental health services can yield greater value for benefit leaders and better health outcomes for the people in their organizations.
Creating an integrated virtual care program may seem like an overwhelming task given all the point solution options available; however, the path to integrated, whole-person care does not need to be complex.
Fueled by strategic mergers with Livongo and MyStrength, a seamless integrated model is available today under one Teladoc Health. Here are a few reasons why benefit leaders should consider it.
Tailored experience and quality, comprehensive care
Integrating virtual care creates a unified experience for everyone. Logistically, there is one application with one login, one registration, and intelligent eligibility matching.
Health education, mental health support and daily wellness reminders are built into the experience, no matter which care service a person primarily uses. Easy, in-app messaging provides a secure channel for clear communication and relationship building with coaches and care providers.
Throughout the experience, a collaborative care team coordinates care across providers, helping to close gaps, guide to the best programs and adapt services as clinical needs change and evolve.
With one of the largest nationwide networks of providers and virtual care across a spectrum of needs, we help keep people safe, and when needed, our intelligent referral process efficiently directs people to in-network providers for additional care and preventive screenings.
Data from Teladoc Health shows that 28% of visits with a Primary360 provider result in a referral to an in-network provider and yields 21% lower spend as a result of efficient provider referrals.
Undeniable positive outcomes
When you deliver these services through a single integrated experience, there is an amplifier effect that improves utilization, retention and follow-up across the experience. Collectively, these factors enable earlier intervention, prevention and better health outcomes.
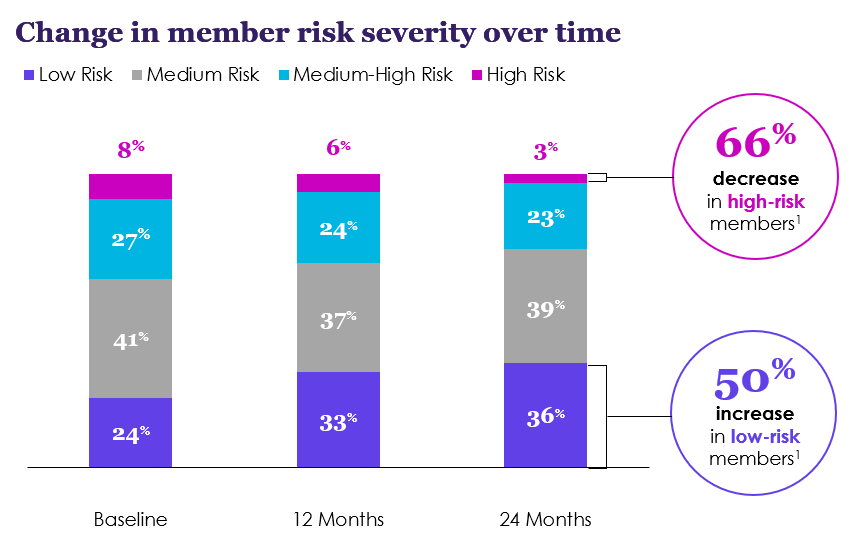
An analysis from our data science team shows enrollment in multiple Teladoc Health chronic condition programs help move populations from high-risk to lower-risk levels. Over the course of two years, severity of disease for diabetes, hypertension and obesity declined 66%, from 8% at baseline to 3% after 24 months, while the number of low-risk members increased 50%, from 24% at baseline to 36% after 24 months.
In addition, Teladoc Health members engaged in mental health and chronic condition services experienced an over 80% improvement in blood glucose, a more than 30% improvement in blood pressure and an over 10% increase in weight loss.
With integrated virtual care, plans also have an opportunity to meet the needs of their entire population and address a spectrum of health needs and challenges. For example:
Support across a wide range of severity levels and conditions, including diabetes, hypertension and weight management.
Services uniquely developed for children and teens with built-in safeguards to ensure parental consent and visibility every step of the way.
Tailored programs for LGBTQ+ mental health and access to providers with experience in gender-affirming care.
Caregiver support and three-way-visits to empower individuals to proactively take part in caring for their loved ones. Single, integrated application also makes it easier, and more likely, for caregivers and parents to seek care for themselves
Access to a diverse network of providers that is sensitive to various life stages, preferences and cultural differences.
Teladoc Health app en Español and on-demand member support in over 240 languages.
Offering integrated virtual care clearly brings numerous advantages to your benefits population. For benefit leaders, an integrated program means less administrative burden, better reporting and improved risk identification and disease prevention. Simple to implement and easy-to-manage integrated virtual care from Teladoc Health drives measurable value and meaningful outcomes for your entire population.
Contact a Teladoc Health representative to learn more about the value your organization can gain by integrating virtual care services.









